Practical Nutrition and Lifestyle Strategies for Managing Diabetes Effectively
Published on July 16, 2025
Understanding Diabetes
Diabetes is predominantly represented as type 1 or type 2 disease, the latter being the most frequent disease worldwide. Type 1 diabetes is due to autoimmune destruction of the beta cells of the pancreas resulting in absolute insulin deficiency. Type 2 diabetes is a combination of insulin resistance (the body's cells do not use insulin effectively) and a relative decline in insulin secretion. The two conditions lead to sustained high blood sugar levels, which in turn damage blood vessels and major organs.
Aside from all of these, since many people may not know gestational diabetes develops during pregnancy and it does require special attention to save both mother and baby. Nonetheless, alternative forms of diabetes have been described that develop from genetic mutations, pancreatic disease, and endocrine disease. Correct diagnosis is necessary in order to provide effective therapy.
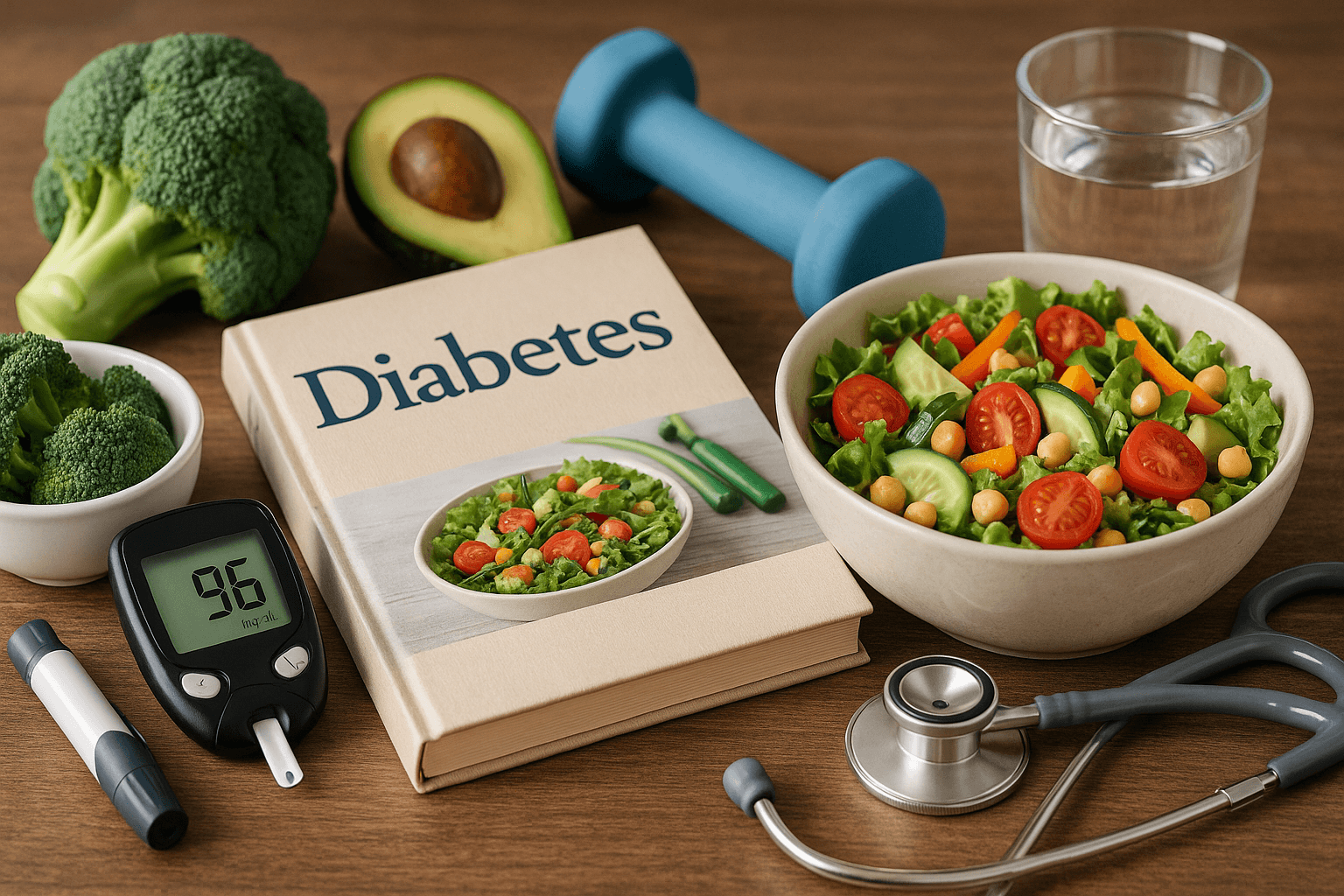
Significance of Early Diagnosis and Screening
Early detection by means of regular screening is critical, especially for those with risk factors including obesity, a family history, age over 45, or membership in some ethnic groups. Conventional diagnostic tools are fasting plasma glucose, oral glucose tolerance tests and glycated hemoglobin (HbA1c) assessment. Early diagnosis enables intervention that can help to delay or even prevent the progression of disease and its complications.
Pregnant women should be screened for gestational diabetes in prenatal care to lower risks for mother and baby.
Nutrition Principles for Diabetes Management
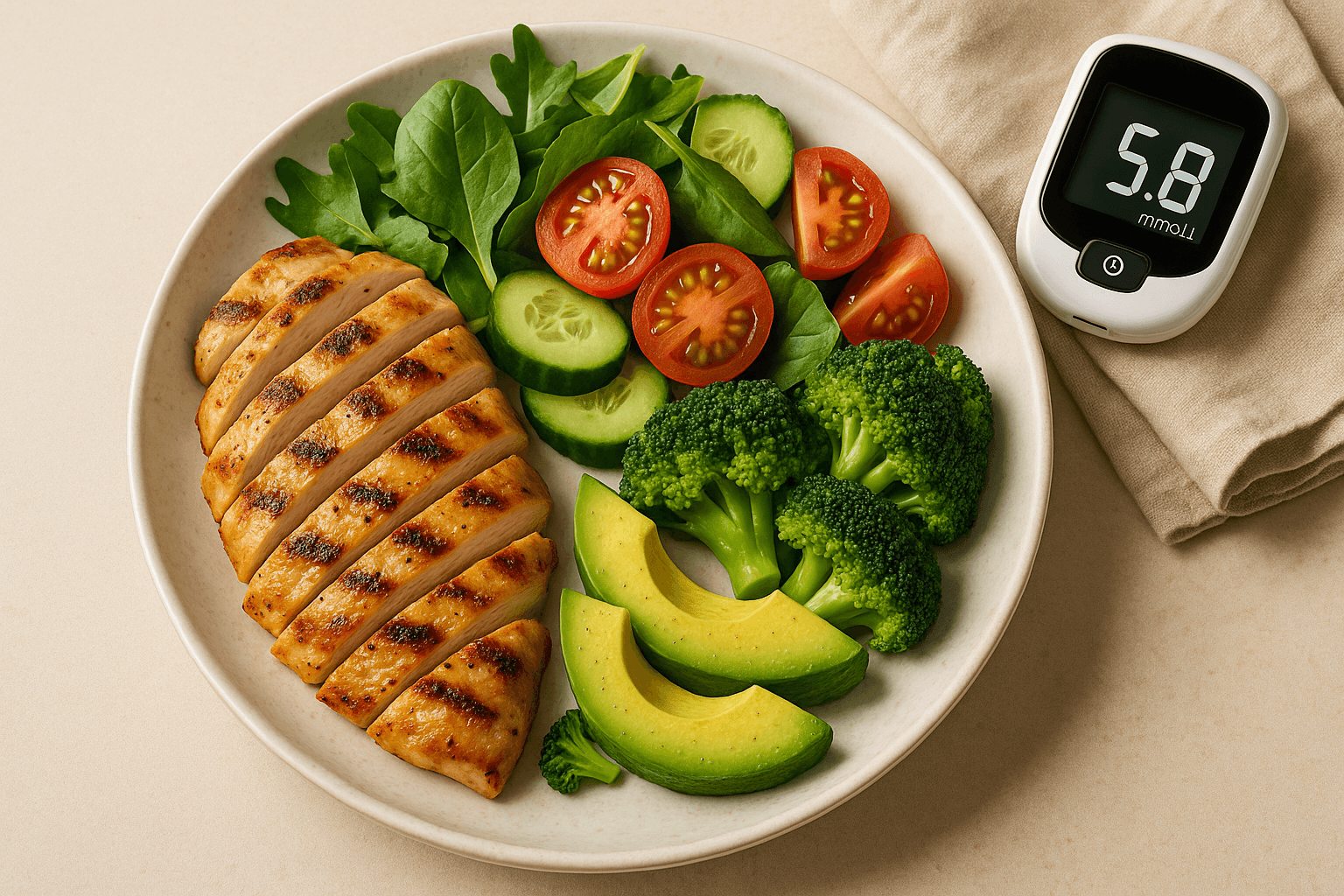
Emphasize Low Glycemic Index (GI) and Glycemic Load (GL) Foods
Eating a low GI and GL diet like legumes, whole grains, non-starchy vegetables, nuts, and most fruits can help prevent quick increases in blood glucose and insulin. These are the type of foods that will cause a gradual rise in blood sugars and do not stress the pancreatic cells that make insulin.
Balancing Macronutrients for Stability
The combination of carbohydrates with protein and healthy fats slows glucose digestion and absorption, leading to increased satiety and control of blood sugar.
Lean proteins, from fish and poultry to legumes and low-fat dairy, help muscle health and metabolism.
Fats from olive oil, avocados, nuts, and fatty fish help protect your heart and contribute to hormone production. Saturated and trans fats should be limited due to their adverse outcomes on health.
Portion Control and Meal Timing
Portion management aids in calorie and carbohydrate control to prevent post-meal spikes. Coordinating meal timing with the body’s internal clock — eating more in the morning and less in the evening — may support weight control and reduce diabetes and heart disease risk.
Increasing Fiber Intake
Soluble fiber in oats, fruits, vegetables, and legumes slows carbohydrate digestion and promotes blood sugar stability. Fiber supports gut microbiome diversity, contributing to metabolic and immune health.
Reducing Processed Foods and Added Sugars
Limiting processed foods, sugary drinks, and snacks lowers inflammation, weight gain, and glucose variability, all of which are associated with diabetes complications.
Hydration and Fluids
Proper hydration supports kidney function and metabolism. Water and non-caloric drinks are encouraged, while sweetened and caffeinated beverages should be minimized.
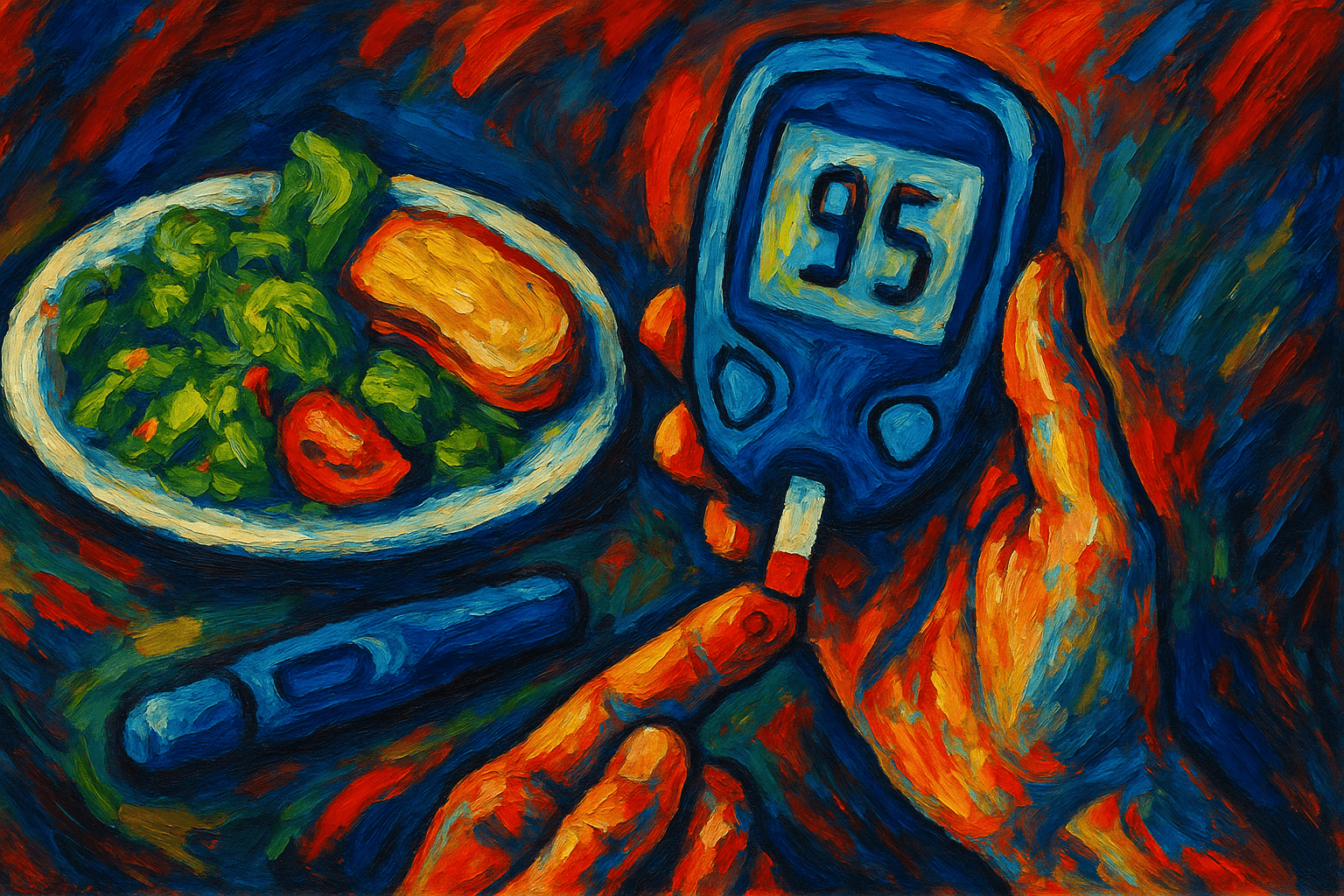
Practical Meal Planning and Preparation
Structured meal planning helps adherence to nutritional goals and reduces impulsive eating.
Batch cooking, pre-portioned snacks, and organized grocery lists enhance convenience and reduce food waste.
Mobile apps and glucose monitors enable personalized feedback and adjustment.
A varied, inclusive diet ensures nutritional adequacy and enjoyment.
Physical Activity: A Vital Component
Aerobic Exercises
Moderate-intensity activities like walking, swimming, or cycling for 150 minutes per week enhance glucose metabolism and cardiovascular health.
Resistance Training
Strength training 2–3 times per week preserves muscle mass, increases metabolic rate, and enhances insulin sensitivity.
Flexibility and Balance
Yoga, Pilates, and stretching improve mobility, reduce injury risk, enhance relaxation, and support mental health.
They also reduce inflammation and improve sleep—key factors for managing diabetes.
Drug Prescription and Technological Developments
Pharmacologic therapies such as metformin, sulfonylureas, SGLT2 inhibitors, GLP-1 receptor agonists, and insulin aid in glycemic control.
Newer agents also provide cardiovascular and renal benefits.
Continuous Glucose Monitoring (CGM) and insulin pumps allow real-time glucose trend analysis and dosage adjustments.
Telehealth and mobile apps are increasing patient empowerment and engagement.
Psychological and Emotional Health Support
Living with diabetes is emotionally taxing. Depression, anxiety, and diabetes distress can impair self-care.
Mental health services, cognitive-behavioral therapy, stress management, and peer support improve adherence and quality of life.
Monitoring and Preventing Complications
Regular screening for complications like retinopathy, nephropathy, neuropathy, and cardiovascular disease is essential.
Meeting glycemic, blood pressure, and lipid targets helps lower morbidity and mortality risks.
Special Populations and Cultural Sensitivity
Pregnant Women: Require individualized dietary and medical management for gestational diabetes.
Children and Youths: Need age-appropriate nutritional plans with family support.
Older Adults: Emphasis on nutrient density, muscle retention, fall prevention, and medication management.
Cultural Considerations: Adapting dietary guidance to cultural food preferences promotes adherence.
Emerging Research and Future Directions
Intermittent fasting, ketogenic and low-carb diets, personalized nutrition (based on genetics and microbiome data), and regenerative medicine are promising strategies.
AI and digital tools are shaping personalized care and self-management.
Factors Influencing Health Status and Access
Access to healthy foods, safe exercise environments, education, and socioeconomic status significantly affect diabetes outcomes.
Public health efforts targeting these determinants are crucial to reduce disparities.
Empowerment Through Education and Self-Management
Patient education fosters self-efficacy and informed decision-making.
Ongoing behavioral counseling and peer support help sustain lifestyle changes and resilience.
Management on a Long-Term Basis and Quality of Life
Effective diabetes management leads to longer life, fewer complications, and improved physical and mental well-being.
Supportive healthcare relationships and adaptation to life changes are key.
Final Thoughts
Diabetes care must be integrative—addressing nutrition, exercise, medication, mental health, and social context.
Empowering individuals through multidisciplinary strategies can lead to healthier, more fulfilling lives.