COMPREHENSIVE GUIDE TO DIABETES: MANAGING BLOOD SUGAR THROUGH NUTRITION AND LIFESTYLE
Published on July 4, 2025
Understanding Diabetes
Diabetes mellitus includes type 1, caused by autoimmune destruction of pancreatic beta cells, and type 2, driven by insulin resistance and impaired insulin secretion. Uncontrolled blood sugar leads to damage of blood vessels and nerves, causing complications like cardiovascular disease, nephropathy, retinopathy, neuropathy, and infections.
Early diagnosis through screening (fasting glucose, OGTT, HbA1c) and prompt treatment improve outcomes. Screening is recommended for adults 45+ and younger individuals with risk factors. Pregnant women should be tested for gestational diabetes.
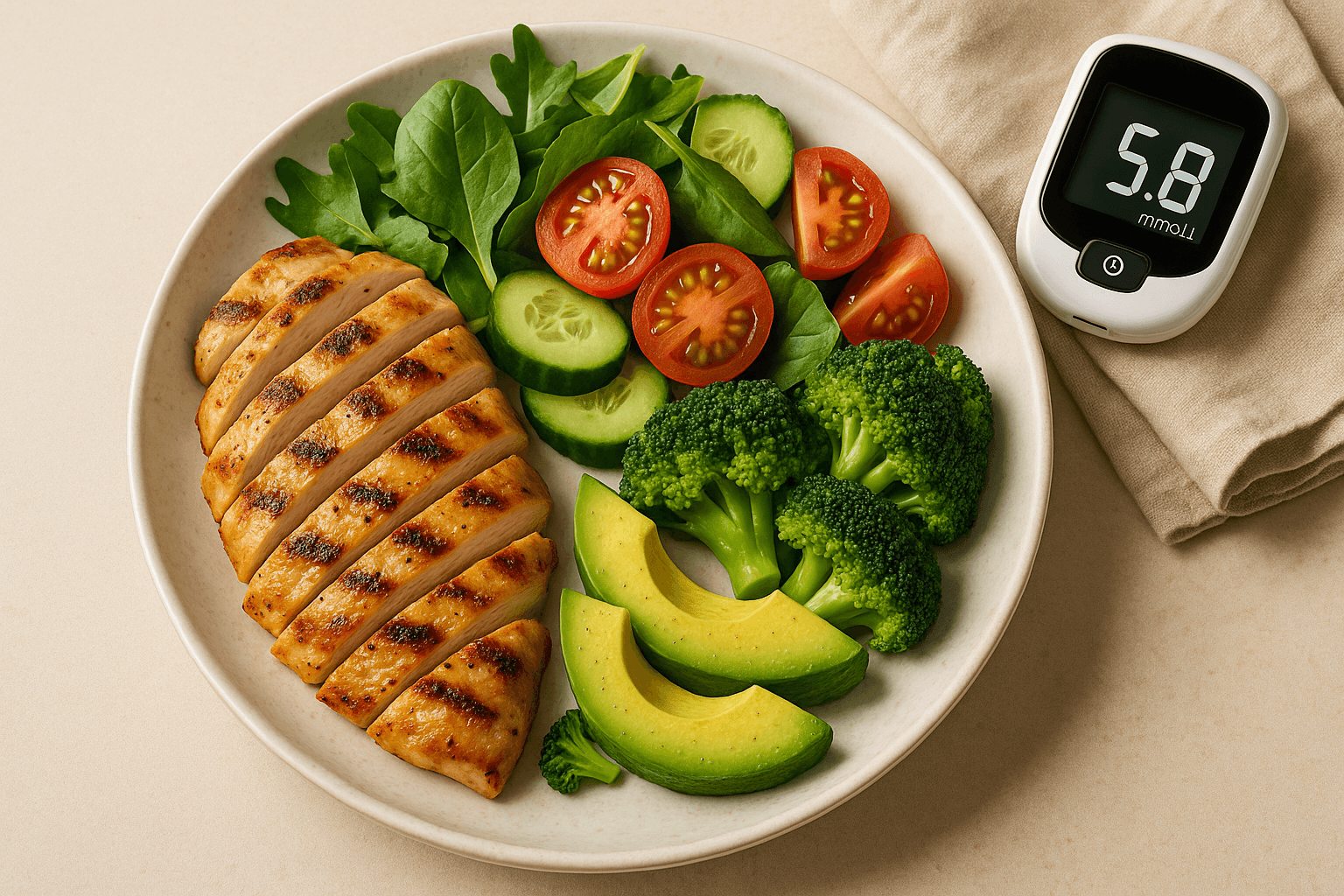
How to Plan Your Diet to Keep Your Sugar in Control
Low Glycemic Index Foods: Beans, whole grains, non-starchy vegetables, and most fruits lower post-meal blood sugar spikes.
Macronutrient Composition: Balance carbs, proteins, and healthy fats. Lean meats, fish, dairy, legumes, nuts, and seeds provide protein. Choose monounsaturated and polyunsaturated fats (olive oil, avocados, fatty fish) while limiting saturated/trans fats.
Fiber Intake: Soluble fiber from oats, legumes, and fruits helps control blood sugar, cholesterol, and supports a healthy microbiome.
Portion Control and Meal Timing: Eat regular meals to prevent extreme blood sugar swings. Align meal timing with circadian rhythms for additional metabolic benefits. Front-loading calories earlier in the day may aid glucose control.
Minimizing Processed Foods and Added Sugars: Avoid sugary drinks, sweets, and highly processed foods, which raise blood sugar and inflammation.
Physical Activity
Exercise improves insulin sensitivity, weight management, and cardiovascular health.
- Aerobic Exercise: Brisk walking, cycling, swimming for 150 minutes/week.
- Strength Training: At least twice weekly.
- Flexibility and Balance: Yoga or stretching to prevent injuries.
Exercise also reduces stress, supporting better blood sugar control.
Medication and Technology
When lifestyle changes aren’t enough, medications like insulin or oral agents (e.g., metformin) are needed. Technologies like CGM and insulin pumps allow precise management. Emerging therapies target genetic pathways for personalized treatment.
Psychological Support
Depression and anxiety can hinder diabetes management. Counseling, mindfulness, and support groups improve adherence and outcomes. Mind-body practices enhance both glucose control and well-being.
Managing Complications
Routine screening for microvascular (retinopathy, nephropathy, neuropathy) and macrovascular (cardiovascular disease) complications enables early intervention. Patient education on symptom awareness and treatment compliance is key.
Special Populations and Considerations
- Pregnancy: Requires specialized monitoring and nutrition for gestational diabetes.
- Children: Nutritional adequacy is critical for growth; family involvement matters.
- Older Adults: Focus on nutrient density, fall prevention, and polypharmacy.
- Cultural Sensitivity: Tailor guidance to cultural dietary preferences to boost adherence.
Emerging Research
Intermittent fasting, low-carb diets, and microbiome modulation show promise in personalizing diabetes care. Research continues into gut microbiome manipulation, beta-cell regeneration, and novel insulin delivery.
Community and Social Support
Support groups, peer mentoring, and community programs increase motivation, knowledge, and mental health, promoting self-management and better outcomes.
Lifestyle Integration and Patient Education
Education about disease mechanisms, self-monitoring, and behavioral strategies enhances motivation and compliance. Culturally relevant education boosts engagement.
Nutrition and Gut Microbiome
Gut microbiota impacts insulin sensitivity and inflammation. Diets rich in prebiotic fibers and fermented foods improve microbiome health, with probiotics and synbiotics under investigation.
Technology and Digital Health
Telemedicine, mobile apps, and wearables improve access and support personalized diabetes management.
Long-Term Commitment and Continuous Learning
Effective diabetes care requires lifelong engagement, ongoing education, and adapting to advances in treatment and nutrition.
Interactions Between Ecology and Health
Access to healthy foods, safe exercise spaces, and healthcare affects diabetes management. Addressing social determinants of health is essential to reducing disparities.
Nutrition and Physical Activity Synergy
Diet and exercise together improve insulin sensitivity, weight control, and cardiovascular health better than either alone.
Sleep and Stress Management
Poor sleep and chronic stress raise blood sugar. Good sleep hygiene and stress-reduction techniques like meditation are integral to holistic care.
Personalized Medicine and Future Directions
Precision medicine, using genetic, metabolic, and lifestyle data, will enable tailored diabetes treatments with fewer side effects.
Final Thoughts
Successful diabetes management requires a person-centered, holistic approach combining nutrition, activity, medication, technology, and psychological support. Empowerment through education promotes long-term health and quality of life.