Practical Nutrition and Lifestyle Strategies for Managing Diabetes Effectively
Published on July 2, 2025
Understanding Diabetes
Type 1: autoimmune destruction of insulin-producing cells → insulin deficiency
Type 2: insulin resistance + possible decreased insulin production → high blood sugar
High blood sugar damages blood vessels & organs → complications like CVD, kidney disease, nerve damage, vision loss
Early detection (symptoms: thirst, urination, fatigue) + early intervention improve outcomes
Nutrition Principles
Choose low-GI carbs: legumes, whole grains, non-starchy vegetables
Pair carbs with protein & healthy fats to slow glucose rise
Control portions to manage total carb intake
Eat plenty of fiber: oats, veggies, fruits, legumes
Avoid processed foods & added sugars → prevent spikes & inflammation
Use healthy fats: olive oil, nuts, fatty fish → support heart health
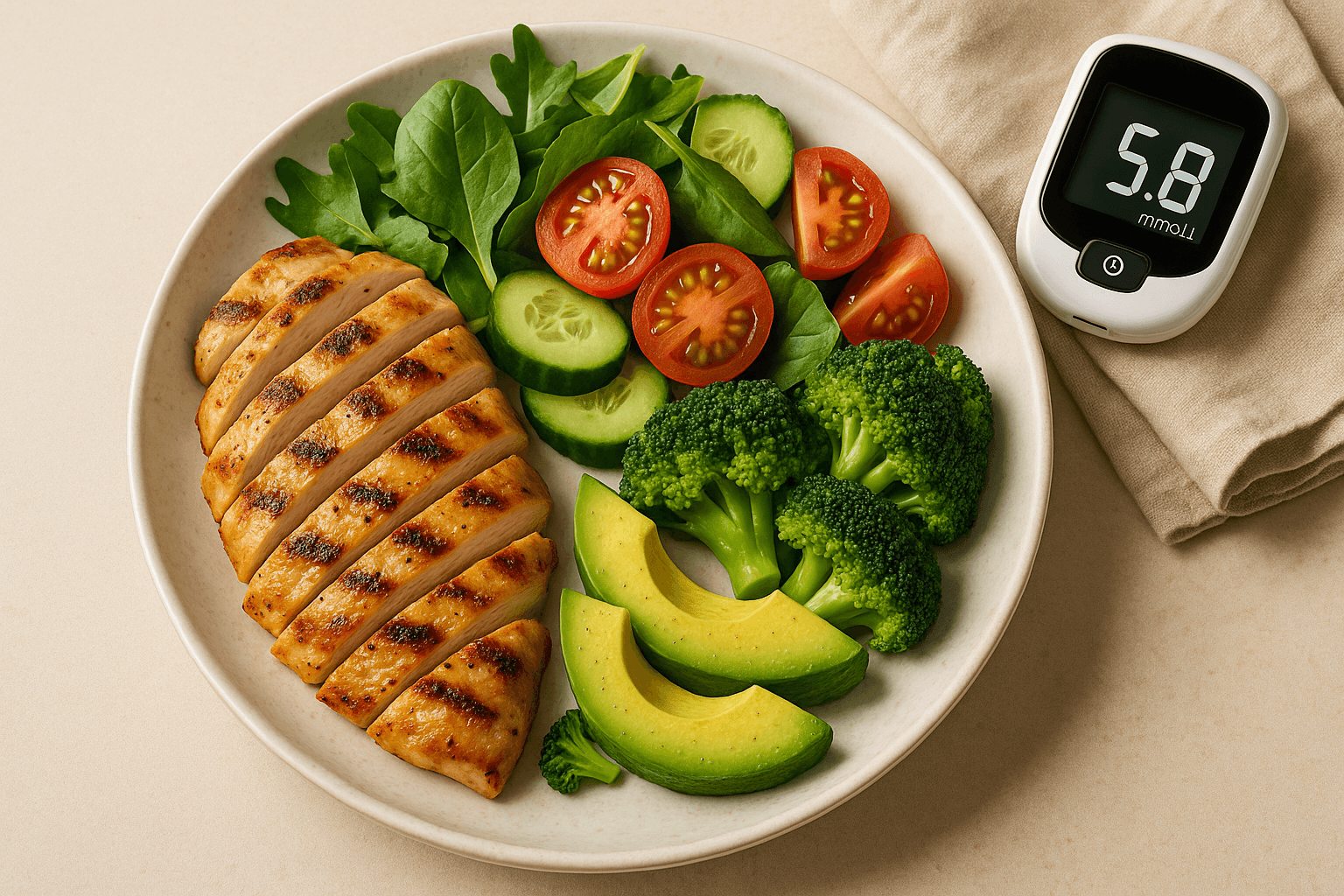
Tailored Diets & Meal Planning
Personalize based on age, activity, medications & culture
Schedule regular meals/snacks to keep blood sugar stable
Use apps & tools for carb counting & tracking
Cook at home for control over ingredients
Read labels & learn carb counting
Physical Activity
At least 150 minutes/week of moderate exercise (walking, cycling)
Include resistance training (weights, bodyweight)
Benefits: improved insulin sensitivity, weight management, lower BP, better lipids
Exercise reduces inflammation & supports mental well-being
Monitoring & Adjustments
Check blood sugar regularly → adjust diet, exercise & medications
Continuous glucose monitoring (CGM) offers real-time feedback
Collaborate with healthcare team for personalized adjustments
Mental Health & Support
Stress, anxiety & depression affect glucose control
Counseling, mindfulness & peer support improve coping & adherence
Emotional health is key for comprehensive diabetes care
Preventing Complications
Control blood sugar, BP & cholesterol with diet + exercise → protect nerves, kidneys, eyes, heart
Routine medical check-ups for early detection of complications
Medications & Technology
Most need meds + lifestyle changes for optimal control
Tools: insulin pumps, CGM devices, smart pens → improve accuracy & convenience
Patient education on proper use is crucial
Special Populations
Pregnancy: manage gestational diabetes for mom & baby health
Children: balanced meals for growth & energy
Elderly: nutrient-rich, easy-to-digest foods to prevent muscle loss
Meal Planning Tips
Regular meals, consistent timing
Mix carbs, protein & fat
Choose whole foods over processed
Plan snacks wisely to avoid lows
Batch cook & meal prep
Emerging Research
Exploring intermittent fasting, low-carb diets & precision nutrition
Genetics & gut microbiome profiling → future personalized diabetes care
Holistic Approaches
Yoga, tai chi, meditation reduce stress & improve metabolic health
Prioritize sleep: 7–9 hrs supports insulin sensitivity
Mindful eating → better choices & glucose control
Community & Social Support
Support groups & community programs boost motivation & control
Sharing experiences improves well-being & adherence
Environmental & Societal Considerations
Increase access to healthy foods & education in communities
Public health efforts can reduce the global diabetes burden
Final Thoughts
Optimal diabetes management blends nutrition, activity, mental health, meds & tech
Education + empowerment = better control & quality of life
Stay informed, seek support & commit to lifelong healthy habits