Diabetes Management: Nutrition Strategies for Better Blood Sugar Control & Long-Term Health
Published on August 26, 2025
Understanding Diabetes & Blood Sugar
Diabetes is a metabolic condition involving impaired insulin action.
Type 1: immune system destroys insulin-producing beta cells → no insulin production.
Type 2: cells resist insulin → high blood sugar.
Chronically high blood sugar damages blood vessels and organs, raising the risk of heart disease, kidney failure, neuropathy, and vision loss.
How Nutrition Impacts Blood Sugar
What you eat directly affects blood glucose. Carbohydrates break into glucose → bloodstream → insulin helps cells absorb it.
In diabetes, insulin secretion or response is impaired → hyperglycemia.
A good diet:
Stabilizes blood sugar
Reduces inflammation
Supports insulin sensitivity
Helps with weight control
10 Practical Strategies for Blood Sugar Management
1. Focus on Low GI Foods Choose foods causing gradual blood sugar rises: whole grains, legumes, nuts, non-starchy vegetables.
2. Balance Macronutrients Pair carbs with protein, fiber, and healthy fats → slows sugar absorption.
3. Practice Portion Control Smaller meals reduce glucose load and prevent spikes.
4. Eat at Regular Times Regular meals maintain stable energy and blood sugar levels.
5. Personalize Your Diet Some people do better with higher protein, others benefit from carb cycling — tailor your plan.
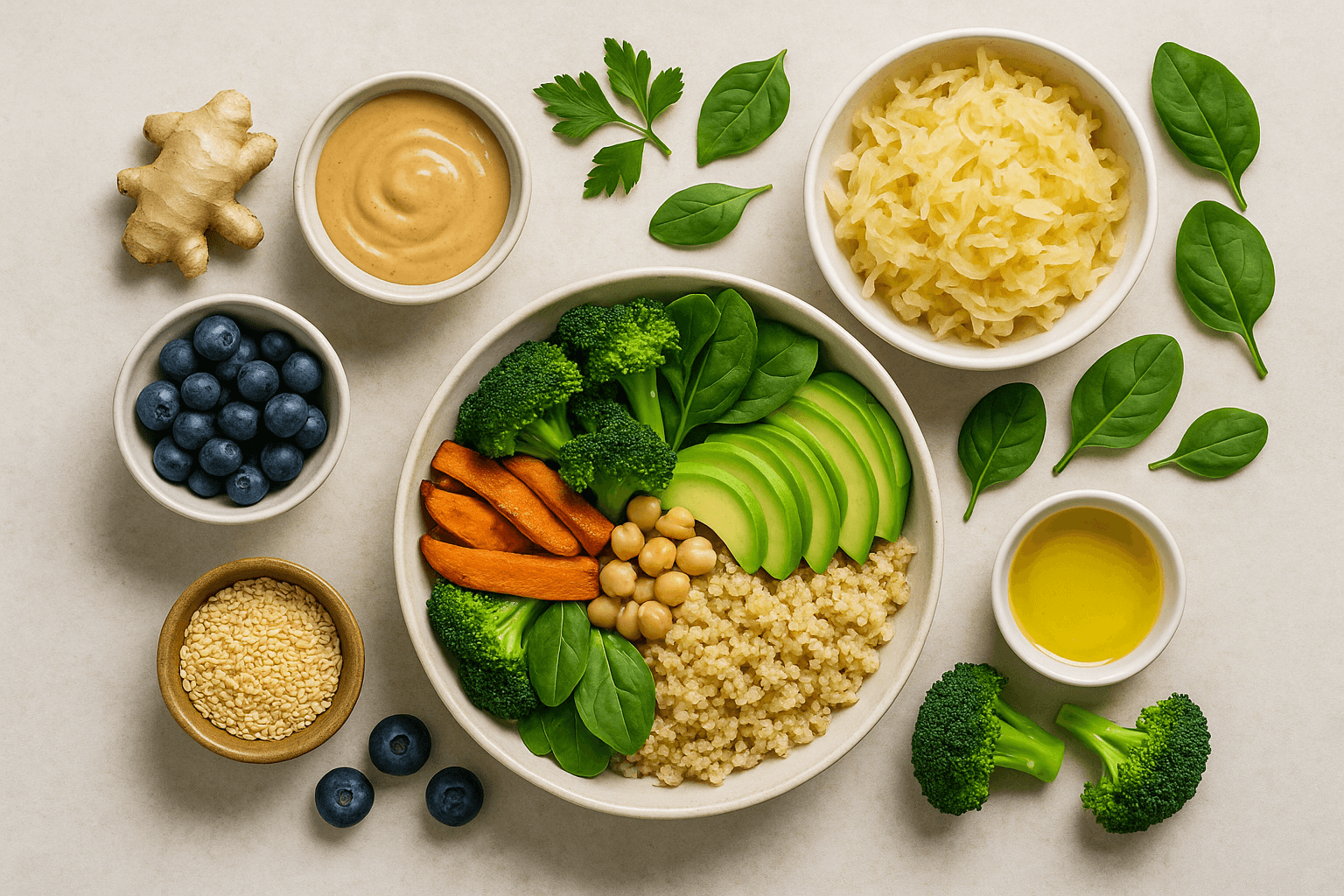
6. Include Anti-Inflammatory Foods Berries, leafy greens, fatty fish, nuts reduce inflammation and improve insulin sensitivity.
7. Support Your Gut Microbiome
High-fiber diets with prebiotics/probiotics enhance gut health → improved glucose metabolism.
Add: kefir, sauerkraut, kimchi.
8. Move More 150 min/week of moderate exercise + resistance training improves insulin sensitivity.
9. Manage Stress Mindfulness, yoga, sleep (7–8 hours) lower cortisol → better blood sugar.
10. Track & Adjust Monitor blood glucose → learn how food, activity & stress impact it. Adjust diet with professional guidance.
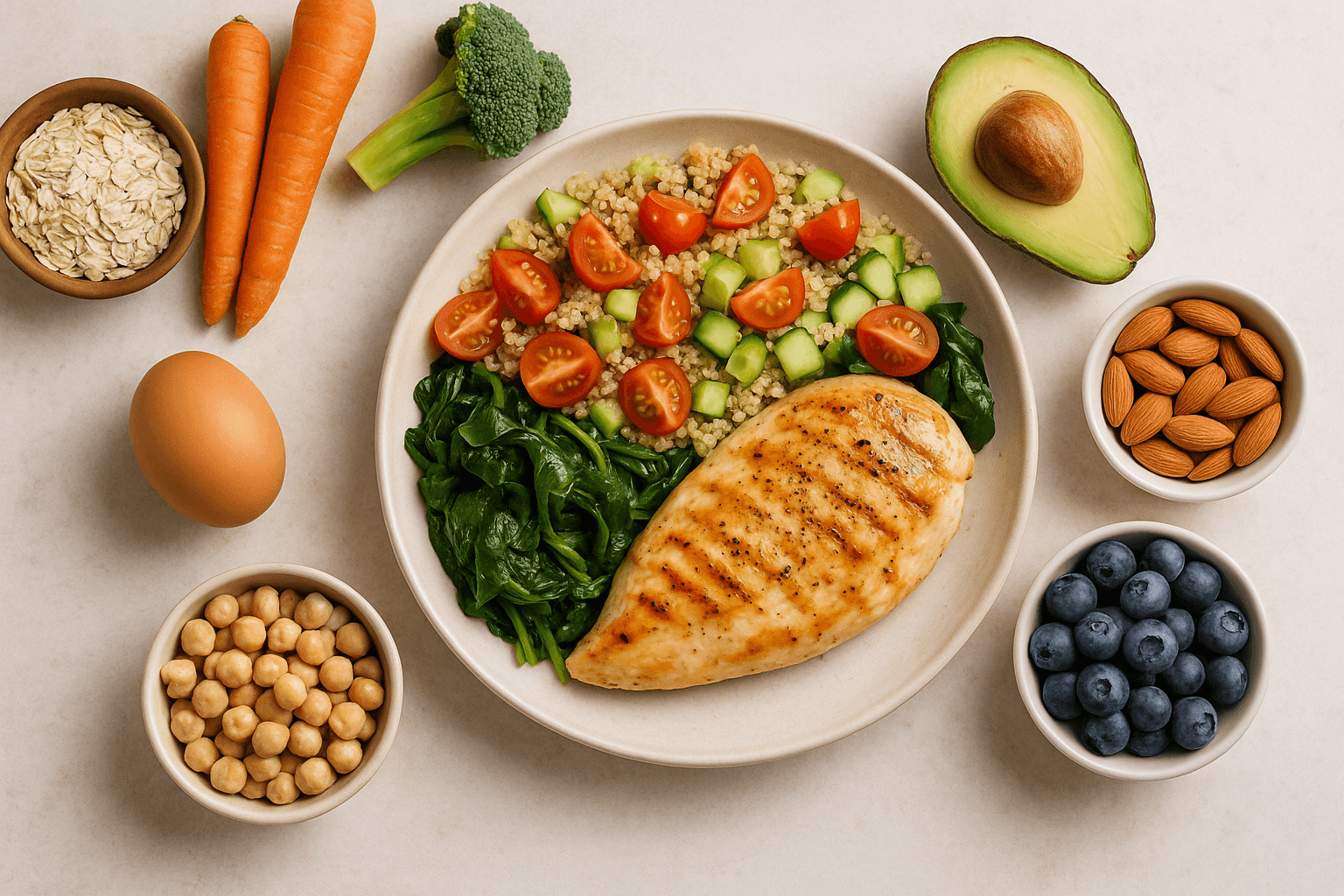
Sample Day for Stable Blood Sugar
Breakfast:
Greek yogurt, chia, strawberries, cinnamon
Lunch:
Quinoa salad with grilled chicken, avocado, greens, lemon-olive oil
Snack:
Almonds + apple
Dinner:
Baked salmon, steamed broccoli, cauliflower rice, sautéed spinach
Myths vs Facts
Myth: Diabetics must avoid carbs completely
Fact: Quality and quantity matter more than abstinence.
Myth: Natural sweeteners are safe in excess
Fact: All sugars affect blood glucose.
Myth: Only overweight people get type 2 diabetes
Fact: Genetics, diet, lifestyle play roles; thin people can develop diabetes.
New Research & Future Directions
Time-restricted eating, intermittent fasting, and personalized nutrition (based on genetics and microbiome profiling) may soon provide tailored approaches to diabetes care.
Final Takeaway
A diabetes-friendly diet isn’t a short-term fix — it’s lifelong, personalized, sustainable. By balancing carbs, eating anti-inflammatory foods, staying active, and reducing stress, you can control blood sugar, lower complications, and lead a healthy, vibrant life.