DIABETES MANAGEMENT THROUGH NUTRITION AND LIFESTYLE STRATEGIES
Published on August 25, 2025
Understanding Diabetes
Diabetes mellitus is a long-term metabolic disorder that affects hundreds of millions globally. Its hallmark is the body’s inability to properly control blood sugar levels. Effective management is essential to prevent complications such as heart disease, nerve damage, kidney failure, and blindness.
Two Types of Diabetes
Type 1 diabetes is an autoimmune condition in which the pancreas produces little or no insulin. Type 2 diabetes is more common and results from insulin resistance and/or progressive insulin deficiency. Both conditions cause elevated blood sugar, which can damage organs and tissues over time.
Other Forms of Diabetes
Gestational diabetes develops during pregnancy. Other rare forms stem from genetics or secondary to illness. Early detection and sustained treatment are key to reducing the severity of disease.
Early Detection and Screening
Screening helps identify at-risk individuals early. Common tests include fasting plasma glucose, oral glucose tolerance test, and HbA1c.
Screening is advised for adults over 45 or younger individuals with risk factors like obesity, family history, or high-risk ethnicity.
Gestational diabetes screening is essential for the health of both mother and child.
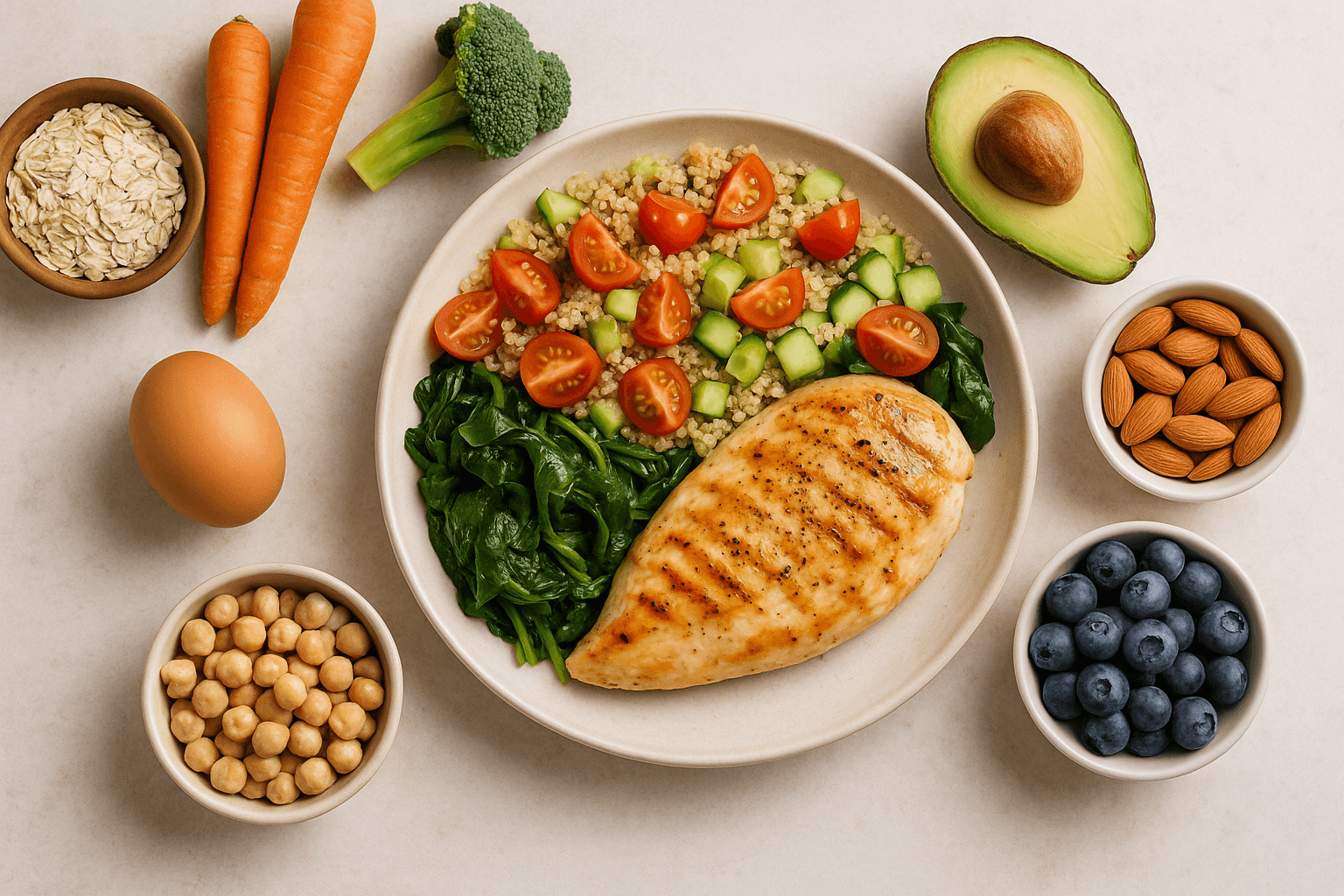
Nutritional Approaches to Stabilize Blood Sugar
Balanced nutrition is the cornerstone of diabetes care.
Low Glycemic Index (GI) and Glycemic Load (GL)
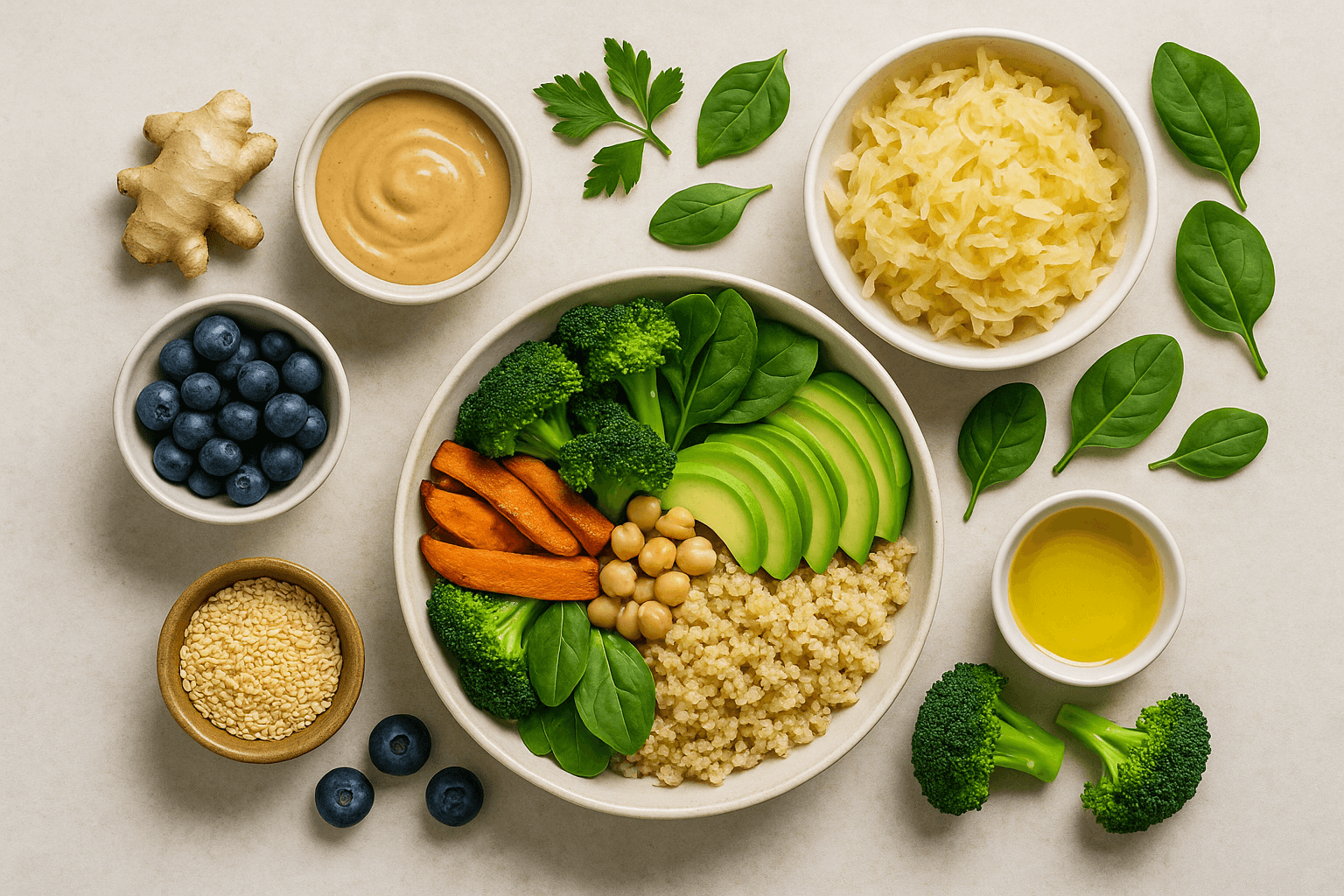
Focus on foods that are slowly absorbed, such as:
beans
whole grains
non-starchy vegetables
many fruits
These minimize blood sugar spikes and reduce insulin demand.
Macronutrient Composition
A balanced mix of carbs, protein, and fats slows digestion and stabilizes blood sugar.
Proteins: lean meats, fish, eggs, legumes, dairy, nuts, seeds
Fats: favor olive oil, avocados, nuts, and fatty fish; avoid trans fats
Plant proteins are also beneficial for heart health.
Fiber Intake
Fiber regulates blood sugar and cholesterol.
Soluble fiber sources: oats, legumes, fruits
Fiber enhances gut health and glucose tolerance.
Portion Control and Meal Timing
Eat regularly (3 meals, 3 snacks) with controlled portions to avoid sugar highs and lows.
Eating more calories earlier in the day may improve glucose control.
Limit Processed Foods and Added Sugars
Avoid ultra-processed snacks and sugary drinks to reduce inflammation and promote metabolic health.
Physical Activity
Exercise increases glucose uptake and improves insulin sensitivity.
Aerobic activity: 150+ minutes/week (walking, swimming, cycling)
Resistance training: twice weekly to preserve muscle and boost metabolism
Flexibility and balance: yoga and stretching improve overall wellness
Exercise also improves mood, reduces stress, and supports sleep quality.
Medication and Technology
When lifestyle changes are not enough, medications such as metformin or insulin may be prescribed.
Technological tools like CGMs and insulin pumps improve precision and quality of life.
Digital tools offer real-time feedback for better self-management.
Psychological Support
Diabetes can lead to distress, depression, and anxiety.
Support may include:
counseling
mindfulness
peer support groups
Emotional resilience is vital to successful long-term care.
Preventing and Managing Complications
Screen regularly for:
retinopathy
nephropathy
neuropathy
cardiovascular disease
Control of blood sugar, blood pressure, and cholesterol is critical.
Patient education aids symptom recognition and adherence to treatment.
Special Populations and Considerations
Gestational diabetes: supports both mother and fetus
Children and adolescents: benefit from family support
Older adults: need to preserve muscle mass and prevent falls
Cultural sensitivity: respects food preferences for better adherence
Emerging Research and Future Directions
Promising strategies include:
intermittent fasting
low-carb diets
precision nutrition based on genetics and microbiome
Research on beta-cell regeneration and immunotherapy shows future potential.
Community and Social Support
Engagement with others builds motivation, reduces isolation, and promotes better care.
Lifestyle Integration and Patient Education
Teaching diabetes pathophysiology, self-monitoring, and lifestyle skills empowers better choices.
Motivational interviewing and behavior therapy encourage adherence.
Cultural sensitivity enhances relevance and impact.
Nutrition and Gut Microbiome
Gut health affects insulin sensitivity and inflammation.
Include prebiotics and fermented foods to promote beneficial bacteria.
Technology and Digital Health
Telemedicine, remote monitoring, and mobile apps provide personalized support.
Wearables and AI-driven analytics help deliver proactive care.
Long-Term Commitment and Continuous Learning
Diabetes management evolves with new research and changing needs.
A growth mindset supports lifelong success.
Environmental and Social Determinants of Health
Food access, safe exercise spaces, and socioeconomic conditions influence diabetes care.
Policy interventions can reduce systemic barriers.
Nutrition and Physical Activity Synergy
Combining healthy eating and exercise boosts insulin sensitivity, weight management, and cardiovascular health.
Sleep and Stress Management
Chronic stress and sleep deprivation worsen blood sugar control.
Mindfulness, relaxation techniques, and good sleep hygiene are essential.
Personalized Medicine and Future Care
Precision medicine tailors treatment to genetic, metabolic, and lifestyle factors, optimizing outcomes and minimizing side effects.
Final Thoughts
Diabetes care must be holistic and individualized.
Combining nutrition, movement, medication, technology, education, and emotional support results in better health and improved quality of life.