DIABETES MELLITUS: A COMPLICATED, CHRONIC METABOLIC DISEASE AND ITS MANAGEMENT
Published on August 25, 2025
Diabetes mellitus is a complicated, chronic metabolic disease that affects millions of people around the world. Optimally managing this condition requires a comprehensive, ongoing strategy targeting both the control of blood glucose levels as well as the prevention or delay of complications and an improved quality of life. This comprehensive review provides evidence-based recommendations on nutrition, physical activity, pharmacological therapy, psychological support, and other lifestyle changes. Collectively, these approaches provide individuals with diabetes with the tools they need to take control of their health and sense of wellbeing with confidence and fortitude.
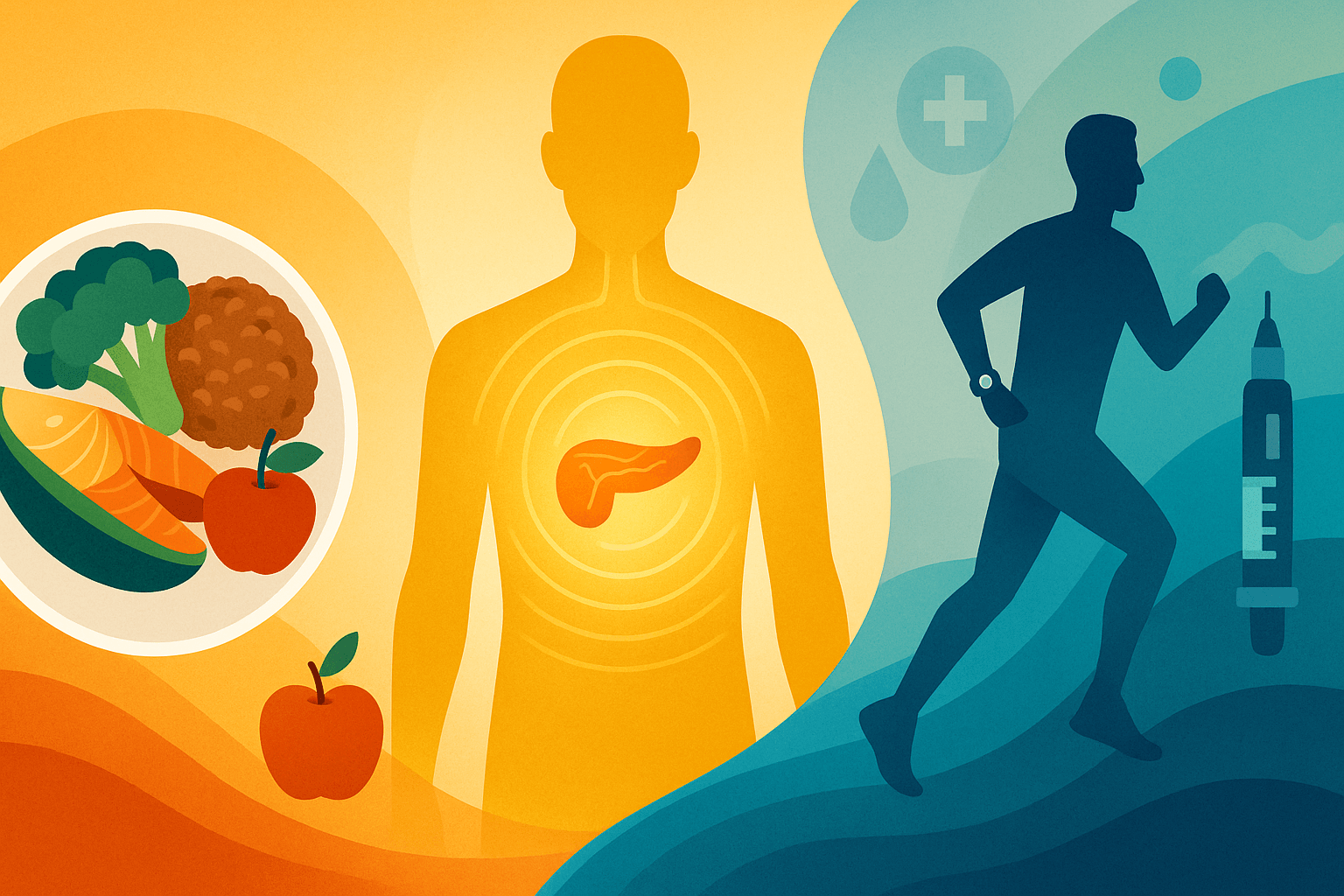
Understanding Diabetes
Diabetes mainly appears as type 1 or type 2 diabetes. Type 1 diabetes is an autoimmune condition in which the body’s own immune system targets the beta cells, which make insulin, in the pancreas and destroys them, causing insufficient production of insulin. People with type 1 diabetes rely on insulin treatment to survive, and they need to monitor their blood sugar carefully.
There are other kinds of diabetes, but type 2, which arises as a result of a mix of a resistance to insulin (where the body’s cells start to ignore it) and declining function of the pancreatic beta cells (since they make less and less insulin), constitutes most of the cases seen worldwide. The sustained hyperglycemia that arises as a long-term consequence, if too poorly controlled, inflicts ongoing harm on the vasculature and multiple organs, contributing to cardiovascular diseases, nephropathy, retinopathy, neuropathy, and lower-limb amputations.
Gestational diabetes, developing during pregnancy, has negative outcomes on maternal and fetal health, and enhances the propensity for the further development of type 2 diabetes in both the mother and child. Other rare diabetes descend on monogenic diabetes and secondary diabetes from pancreatic or endocrine diseases need specific diagnostic and therapeutic strategies.
Timeous and reliable diagnosis with tests such as fasting plasma glucose, oral glucose tolerance test and glycated haemoglobin (HbA1c) is essential in order to commence early and adequate therapy, which will prevent complications.
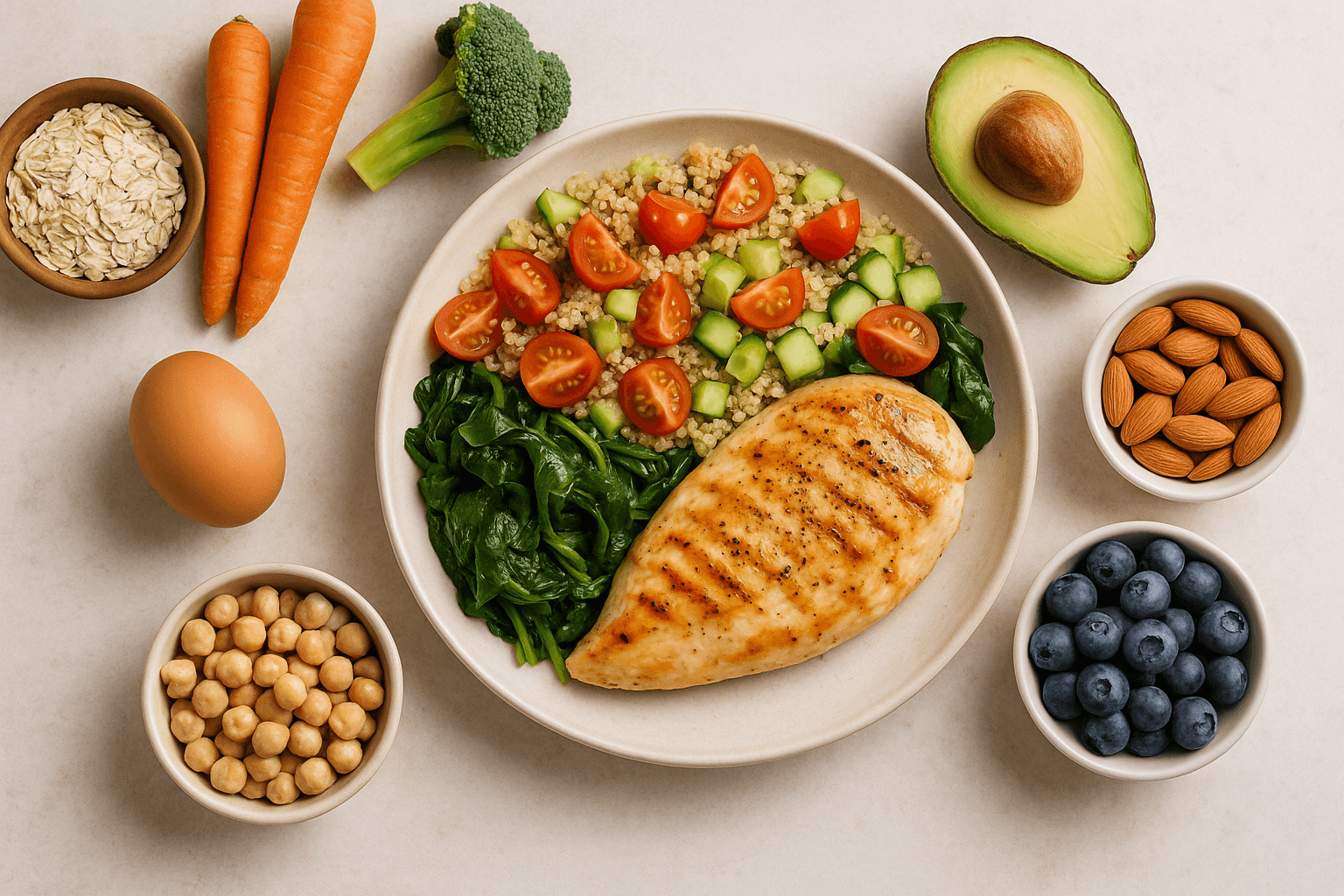
Nutrition Principles for Diabetes Management
Diabetes care is based on nutrition. Appropriate dietary selections contribute to the regulation of blood glucose in control ranges, and prevent cardiovascular risk factors of metabolic syndrome.
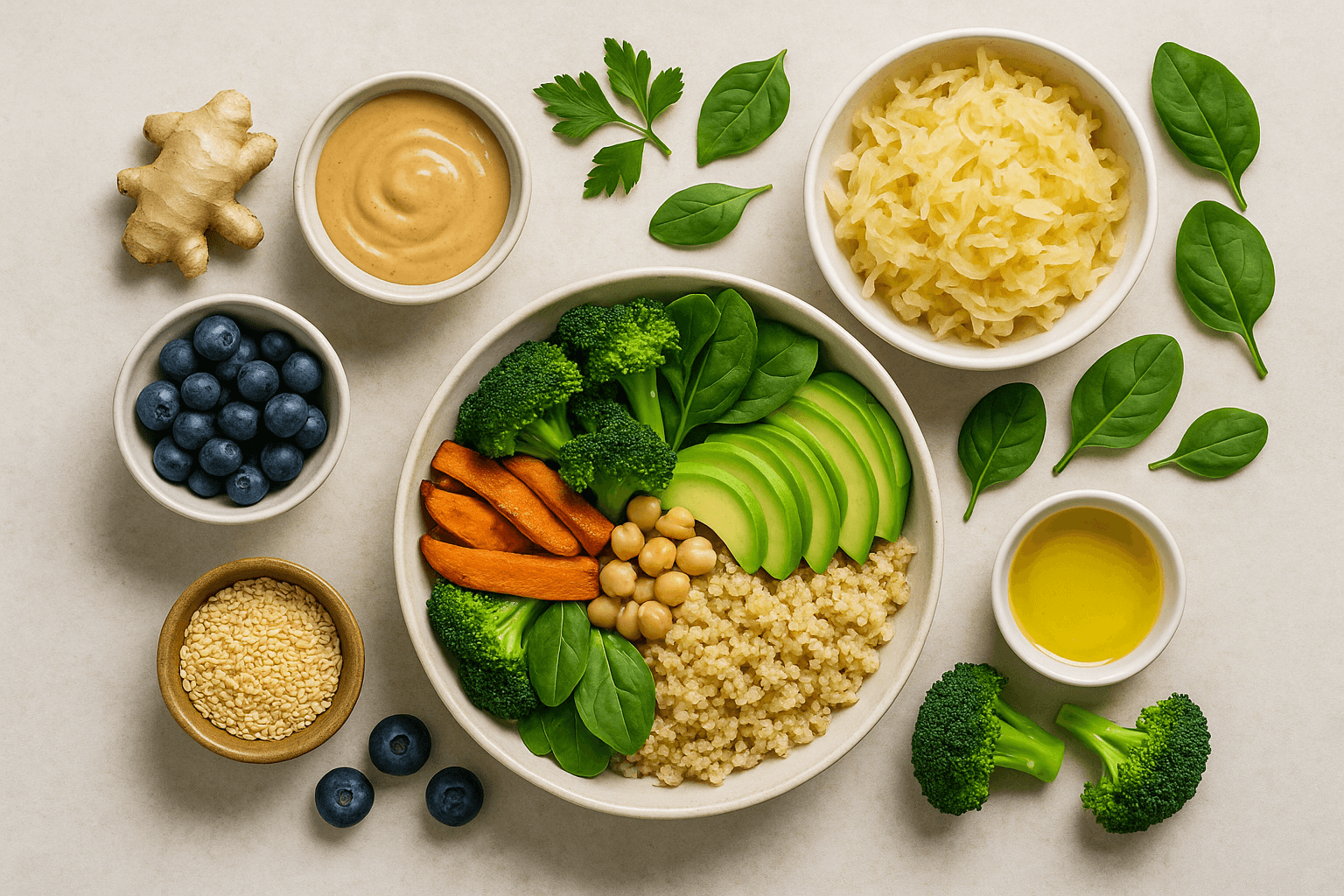
Low GI and Low GL
Choosing low GI and GL foods – such as legumes, whole grains, most fruits, and non-starchy vegetables – results in a slow, steady rise in blood glucose following a meal. This helps keep insulin release steady, decreases the metabolic stress put on pancreatic cells, and helps to prevent large blood sugar surges.
Macronutrient Balance
An organized meal plan that includes carbohydrates, protein, and good fats in appropriate proportions to control digestion and reduce hunger, as well as to regulate the way meals are absorbed is part of an ideal eating pattern. Protein rich foods from meat, poultry, fish, eggs, dairy, legumes, nuts and seeds help repair tissue and maintain muscle. Good fats from olive oil, avocados, some nuts and fatty fish, are known for heart and hormonal health. Reducing consumption of saturated and trans fats is necessary to minimize the risk of cardiovascular disease.
Portion Control and Meal Timing
Portion size management helps to control caloric intake and carbohydrate consumption and to avoid postprandial hyperglycemia. Regular meal timing and circadian organisation of the metabolic process. Research indicates that eating more of our daily calories earlier in the day can improve our sensitivity to insulin and regulation of glucose.
Dietary Fiber
Consumption of dietary fiber, soluble dietary fiber in particular, is associated with increase in the sensitivity of the insulin receptor, reduced serum concentration of LDL cholesterol, preservation of gut microbiota diversity, and enhancement of satiety. Examples include oats, fruits, vegetables, and legumes.
Try to Limit Processed Foods and Added Sugars
It doesn't hurt that restricting processed foods, sugary drinks, and refined grains also lowers chronic inflammation and calorie surpluses, as well as the wild blood sugar swings that drive diabetes onward.
Hydration
Proper hydration helps the kidneys, digestion, and metabolism. Choose water or unsweetened drinks and limit sugary drinks and too much caffeine.
Meal Planning and Preparation
A meal plan encourages eating a more controlled diet and prevents spontaneous meals and unhealthy snacks. Time-saving and time-management practices like batch cooking, meal prep, and creating organized grocery lists minimize time spent in the kitchen, save money, and minimize wasted food. Adding variety helps avoid a boring diet and helps obtain all the nutrients you need.
Utilising online and mobile applications may assist in monitoring food intake and glucose responses to meals, which may enable personalised dietary manipulation.
Physical Activity
Exercise is one of the best ways to manage diabetes. It increases the sensitivity of insulin, helps keep the heart healthy, maintains a healthy body weight, and helps your mood.
- Aerobic Exercise: Do at least 150 minutes a week of moderate-intensity aerobic activity – such as cycling or fast walking – or 75 minutes a week of vigorous-intensity aerobic activity, such as running or a game of singles tennis. Aerobic workouts help muscles consume glucose and bolster heart and lung function.
- Resistance Training: Add strength training workouts 2-3 times per week to help preserve and grow muscle mass, raise basal metabolic rate and insulin sensitivity.
- Flexibility and Balance Exercises: Include yoga, stretching and balance exercises to increase flexibility, decrease risk of injury and improve mental health.
Furthermore, exercise can lower stress hormones and encourage better sleep, two important factors for regulating the metabolism that are often neglected.
Medication and Technological Advances
Pharmacologic interventions such as metformin, sulfonylureas, SGLT2 inhibitors, GLP-1 receptor agonists, and insulin are still necessary for many patients. Novel agents provide cardiovascular and renal benefit beyond glucose reduction.
With innovative tools like continuous glucose monitoring (CGM) and insulin pumps, the real-time measurement of glucose is improving accuracy and patient quality of life. The platforms for telemedicine enhance access for individualized care.
Psychological and Emotional Support
Diabetes related psychological issues such as depression, anxiety and diabetes distress can also pose an obstacle to self-management and glycaemic control among individuals with diabetes. Incorporating mental health offerings including counseling, cognitive behavioral therapy, mindfulness training, and peer support enhances coping, adherence, and well-being.
Monitoring and Preventing Complications
It is important to screen for microvascular complications, including retinopathy, nephropathy, and neuropathy, and macrovascular disease. Active surveillance interventions, if detected early, may help avoid advancement. Appropriate blood glucose, blood pressure and lipids targets mitigate morbidity and mortality.
Education of the patient about symptom identity and symptom-treatment adherence promotes empowerment and proactive management.
Special Populations and Culturally Sensitive Considerations
- Pregnant Moms: Gestational diabetes demands special dietary and medical attention to protect the health of mother and baby.
- Children and Teens: Nutritional interventions require growth and development support and include a family-based component.
- Older Adults: Focus on nutrient-rich diets, preventing falls, cognitive health and mindful use of multiple medications.
- Cultural Adaptation: Customizing dietary advice to cultural preferences and habits enhances compliance and results.
Emerging Research and Future Directions
New promising avenues in addition to the traditional pharmacological are well represented from early-stage approaches, including intermittent fasting, as well as ketogenic and low carbohydrate diets, to personalized nutrition based on genetic and microbiome profiles and regenerative therapies.
Artificial intelligence and digital health tools allow for personalized care and self-management.
Socioeconomic and Environmental Determinants of Health
There is a clear and growing evidence base that access to healthy foods, safe places for physical activity, health care and education, and various socioeconomic factors are important determinants of diabetes outcomes. The action on these determinants by public health policies and community-based programs is important for the equitable provision of healthcare.
Long-Term Empowerment and Self-Management
The long-term control of diabetes requires ongoing education, behavioral support, and lifestyle adjustments. Enabling patients to take an active role in care decisions forges resiliency and leads to better health.
Final Thoughts
Achieving optimal diabetes control requires a holistic, multidisciplinary approach that includes nutritional, exercise, medication, psychological, and social determinants of health. With continued learning and individualized management, patients can attain the best possible glycemic homoeostasis, avoid complications and fulfil themselves.