Mastering Blood Sugar: What a Balanced Diet Really Looks Like for People with Diabetes
Published on June 11, 2025
Managing diabetes isn’t about cutting sugar completely — it’s about smart choices, structure, and cooking meals that give energy, satisfaction, and stability. Let’s explore what real balance looks like on your plate.
The Essence of a Diabetes Diet
For type 1, type 2, or prediabetes, nutrition goals include:
Regulating blood sugar
Supporting healthy weight
Reducing cardiovascular risk
Providing essential nutrients
Improving insulin sensitivity
Preventing complications (neuropathy, kidney disease, etc.)
Food is medicine — and a form of self-care.
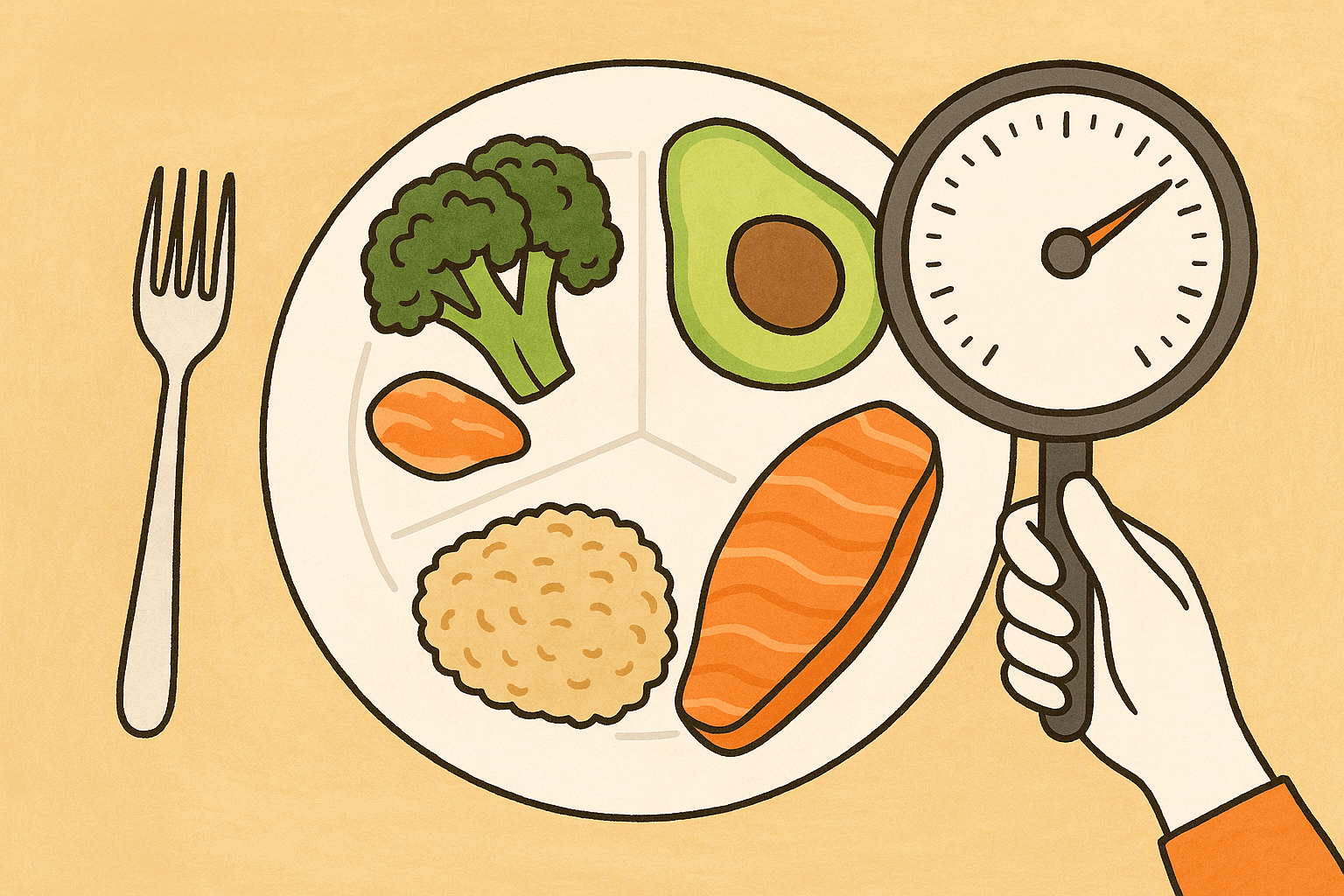
Balanced Plates: The Foundation
Use the plate method:
Half: non-starchy vegetables (spinach, zucchini, cauliflower, mushrooms)
Quarter: lean proteins (chicken, fish, eggs, tofu, legumes)
Quarter: complex carbs (quinoa, brown rice, sweet potatoes, lentils)
Add: healthy fats (avocado, olive oil, tahini, nuts, seeds)
Why it works:
Fiber slows glucose absorption
Protein boosts satiety and preserves muscle
Fat aids vitamin absorption and hormone production
Pro tip: Use a 9-inch plate to prevent oversized portions.
Carbs Aren’t Evil — It’s All About Type and Timing
Carbs impact glucose the most, but the right kind — in the right amount — can work with your body.
Smart carbs:
Whole grains (oats, quinoa, farro)
Tubers (beets, carrots, sweet potatoes)
Legumes (chickpeas, lentils, black beans)
Fruits (berries, apples, citrus)
Pairing matters:
Oats + walnuts + yogurt
Whole grain toast + avocado + egg
Chickpeas + sautéed greens + tahini
Portion rule: Start with ½ cup cooked grains.
Timing tip: Larger carb portions are best earlier in the day.
Choose low/moderate glycemic index foods to limit spikes.
Don’t Skip Meals — Plan Them
Aim for:
3 consistent meals daily
1–2 snacks if needed (especially with insulin)
Balanced breakfast ideas:
Berry chia Greek yogurt
Veggie omelet + whole grain toast
Green smoothie + nut butter + protein powder
Snack ideas:
Celery + peanut butter
Carrot sticks + hummus
Cottage cheese + cucumber
Evening rule: Finish dinner 2–3 hours before sleep to aid overnight glucose control.
Hydration and Hidden Sugar
Water supports glucose excretion and overall metabolism. Drink more when:
Eating more fiber
Being active
Taking dehydrating meds (e.g. metformin)
Watch for sugar traps:
Bottled smoothies
“Low-fat” yogurts
Granola bars
Sweetened nut milks
Hydration tips:
Infuse water with lemon, cucumber, mint
Herbal tea and sparkling water are great no-sugar options
Monitor caffeine, which can raise blood sugar in some
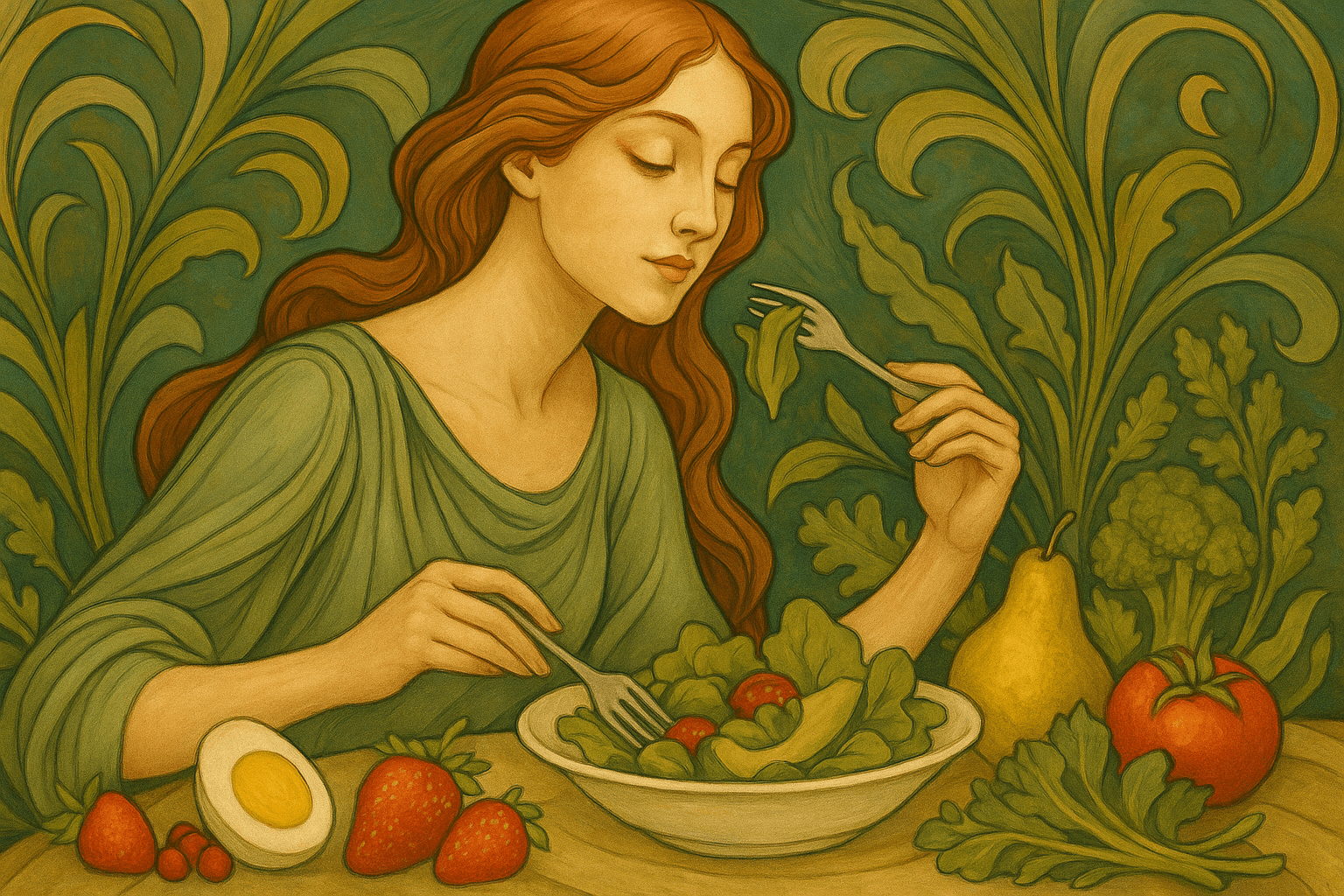
Mindful Eating = Better Glucose Control
Habits to practice:
Eat without screens
Use smaller plates
Chew slowly and rest fork between bites
Use a timer (15–20 min per meal)
Take a moment to feel gratitude before eating
Stress raises cortisol, increasing insulin resistance. A calm eating environment supports better digestion.
Micronutrients That Matter
Key nutrients for blood sugar management:
Magnesium — improves insulin sensitivity (leafy greens, seeds)
Chromium — helps glucose regulation (whole grains, broccoli)
Vitamin D — aids insulin function (test and supplement as needed)
Omega-3s — reduce inflammation (fish, flax, walnuts)
Note: Metformin may deplete B12 and zinc. Check with your doctor.
Fiber goal: 25–35g/day
Soluble fiber (in oats, legumes, apples) slows sugar absorption
Potassium (beans, avocados, greens) supports heart and kidneys
Always speak to a healthcare provider before starting supplements.
Final Words
Managing diabetes with food is about structure — not suffering.
Meals should be energizing, nourishing, and enjoyable.
Listen to your body. Adjust portions based on your glucose responses.
Find meals you enjoy and build consistency around them.
Remember: Eating well isn’t punishment. It’s your path to strength, vitality, and lasting freedom.